Food allergies are growing as a national public health concern. The Centers for Disease Control and Prevention (CDC) stated in 2008 that the prevalence of a reported food allergy increased 18 percent among children younger than 18 years from 1997 to 2007. More recently, a study of emergency room visits and hospital admissions in Illinois due to anaphylaxis (a severe, life-threatening, allergic reaction) occurring among children and induced by food found that such visits and admissions increased annually by 29.1 percent from 2008 to 2012. Consulting our FAIR Health database of over 23 billion privately billed health care procedures, we sought to shed light on recent trends and patterns in food allergies and the anaphylactic reactions that can result from them.
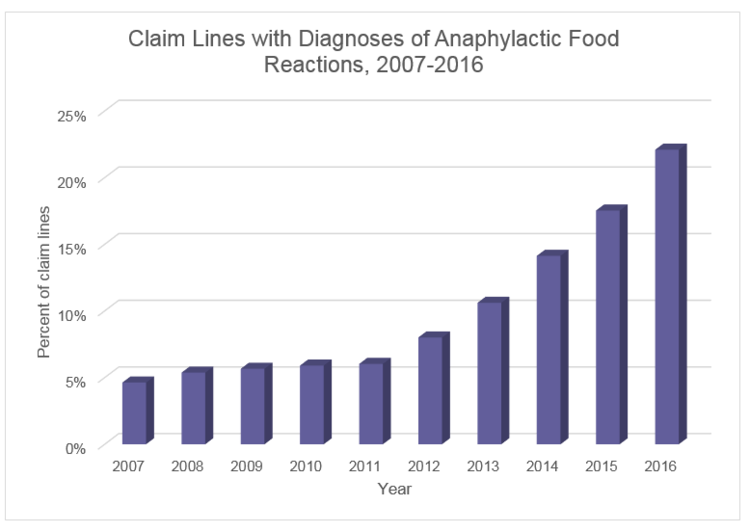
As seen in the chart below, private insurance claim lines (the individual procedures or services listed on an insurance claim) with diagnoses of anaphylactic food reactions climbed 377 percent nationwide from 2007 to 2016. (“Percent of claim lines” in the charts below is the percent of all claim lines associated with a given diagnosis, such as anaphylactic food reaction, in a given time period, such as 2007-2016).
A variety of foods can cause allergic reactions, and sometimes the food is not identified at the time of diagnosis. When the claim lines with diagnoses of anaphylactic food reaction were analyzed by type of food, the most common reaction (33 percent of claim lines) was associated with “other specific foods,” which generally means that the actual allergy is not known, prompting the physician to use a generic diagnosis code. Among specifically identified foods causing anaphylaxis, the most common were peanuts (26 percent), followed closely by tree nuts and seeds (18 percent). Egg allergies, crustacean allergies (e.g., allergies to shrimp or lobster) and dairy allergies were also common, making up, respectively, 7 percent, 6 percent and 5 percent of the anaphylactic food reaction claim lines.

Interestingly, in 2016, the incidence of billing with the “other specific foods” diagnosis code decreased, which was probably due to better training in the ICD-10-CM set of diagnostic codes and the great quantity of educational information about food allergies that has been disseminated over the years. Claim lines associated with anaphylaxis due to “other specific foods” did not increase as much as anaphylactic food reactions attributed to a specific food or food category, with only a 71 percent increase from 2007 to 2016. By comparison, claim lines with diagnoses of peanut anaphylactic reactions increased 445 percent and those with diagnoses of tree nuts/seeds anaphylactic reactions increased 603 percent.

Claim lines with diagnoses of a history of food allergy increased in both urban and rural populations from 2007 to 2016, although with a decrease in both populations in 2016. Despite evidence from other researchers that childhood food allergies are more prevalent in urban than rural areas, our data show that the increase in claim lines with diagnoses of a history of food allergy was greater in rural (110 percent) than urban (70 percent) areas.

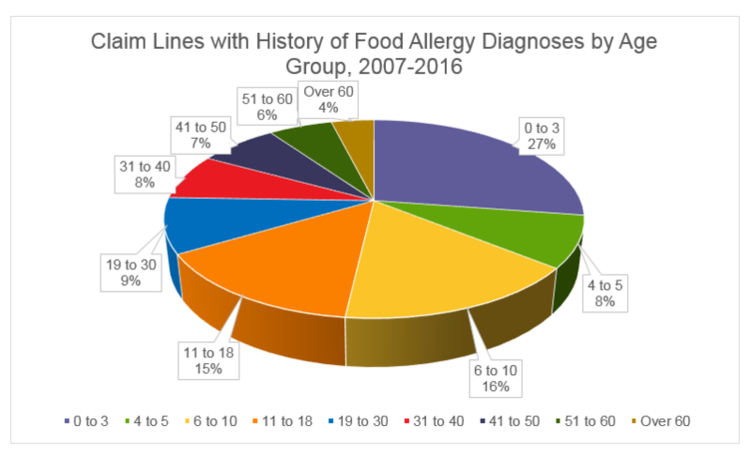
Food allergies are commonly thought of as a childhood condition, but for some children, food allergies continue into adulthood, and adult-onset food allergy does occur. Our data suggest that food allergies are predominantly, but not exclusively, found in young people. Almost a third (27 percent) of all claim lines with diagnoses of a history of food allergy were attributable to patients between the ages of 0 and 3. Preschool age children (4-to-5-year-olds) accounted for 8 percent of the total, with individuals between the ages of 6 and 18 making up an additional third (31 percent). Altogether, patients 18 years old and younger accounted for 66 percent of the claim lines, those over 18 years old the remaining 34 percent.
Many questions about food allergies remain unanswered, and we hope to continue to study this issue. Indeed, in the coming months, we plan to issue a white paper that will delve into such aspects of food allergies as gender, the relationship between specific food allergies and age, geographic distribution, treatments and costs. Such research, in turn, may inspire other researchers and help to inform policy or protocols about this serious and growing health condition.
Robin Gelburd, JD, is the president of FAIR Health, a national, independent, nonprofit organization with the mission of bringing transparency to health care costs and health insurance information. FAIR Health oversees the nation’s largest collection of health care claims data, which includes a repository of over 23 billion billed medical and dental procedures that reflect the claims experience of over 150 million privately insured individuals, and separate data representing the experience of more than 55 million individuals enrolled in Medicare. Certified by the Centers for Medicare & Medicaid Services (CMS) as a Qualified Entity, FAIR Health receives all of Medicare Parts A, B and D claims data for use in nationwide transparency efforts.



